
U.S. Health Insurance Market Size, Share, Trends and Forecast by Provider, Type, Plan Type, Demographics, Provider Type, and Region, 2026-2034
Market Overview:
The U.S. health insurance market size was valued at USD 469.8 Billion in 2025. Looking forward, IMARC Group estimates the market to reach USD 641.1 Billion by 2034, exhibiting a CAGR of 3.50% from 2026-2034. The escalating demand for private health insurance policies, increasing costs of healthcare services, and the rising need for comprehensive health insurance coverage among the masses across the United States are some of the factors impelling the growth of the market.
|
Report Attribute
|
Key Statistics
|
|---|---|
|
Base Year
|
2025 |
|
Forecast Years
|
2026-2034
|
|
Historical Years
|
2020-2025
|
| Market Size in 2025 | USD 469.8 Billion |
| Market Forecast in 2034 | USD 641.1 Billion |
| Market Growth Rate (2026-2034) | 3.50% |
Access the full market insights report Request Sample
The market is experiencing steady growth because of increasing costs of healthcare services and heightened demand for comprehensive health insurance coverage among the masses. This is encouraging people to seek ways to reduce financial burdens across the United States. The heightened costs related to medical services, treatment, and hospitalization are making more people invest in health insurance plans that provide broad and inclusive coverage. Additionally, there is a rise in the awareness and demand for value-based care, which focuses on patient outcomes rather than the volume of services provided. The growth of accountable care organizations (ACOs) and bundled payment programs is driving this trend in the country, where insurers incentivize healthcare providers to deliver high-quality, efficient care.
The rising demand for private health insurance because of its customizable coverage and technological advancements to improve insurance platforms are supporting the market growth in the country. Technological advancements are allowing insurance providers to offer more personalized plans that cater to the specific needs of patients. Digital platforms enable policyholders to compare plans, manage benefits, and receive tailored Wellness recommendations. The demand for more transparency and simplified user experiences is encouraging insurers to adopt tools that foster better understanding and engagement, contributing to more informed decision-making among people. Insurers are increasingly focusing on preventive care services as a means to reduce long-term health care costs. Coverage for routine checkups, screenings, and Wellness programs encourages early detection and management of health issues, which can result in lower expenses over time.
U.S. Health Insurance Market Trends:
Rising Costs of Healthcare and Need for Comprehensive Coverage
The continuous rise in healthcare expenses is driving the need for extensive insurance among people in the United States. According to a report published by Reuters, it is seen that healthcare expenditures in the United States increased by 7.5% in 2023, reaching $4.8 trillion. The main reason for this trend is the increased expenses of medical services, medications, and long-term care. Recently, the increasing need is promoting rivalry among insurance companies, encouraging them to be creative and broaden their range of services. The increase in long-term illnesses like diabetes and heart problems is driving the demand for health insurance plans that include more services, like specialized treatment and ongoing check-ups. In general, the rising costs of healthcare and the desire for affordable yet comprehensive coverage are influencing the direction of the market, emphasizing the importance of health insurance for both financial and physical health.
Rising Private Health Insurance Demand
Private health insurance is witnessing robust growth, fueled by increasing healthcare costs and demand for customizable coverage. With the limitations of public programs, individuals are turning to private insurers for shorter wait times, specialized care, and advanced facilities. Additionally, the inclusion of wellness incentives, such as gym memberships and preventive care discounts, attracted a health-conscious audience. This sector’s rise illustrates the evolving preferences of Americans, emphasizing flexibility and personalization in health insurance offerings. In October 2024, Aetna declared the launch of SimplePay Health, a novel health plan with no deductibles curated for self-insured employers. This new health plan provides employees with one monthly bill that summarizes all of their medical and pharmacy claims for the prior 30 days.
Technological Innovations in Insurance Delivery
The market is benefiting from technological advancements that increase accessibility and efficiency. Besides this, leading insurance businesses are recently implementing artificial intelligence (AI)-powered solutions to increase customer interaction, reduce administrative burden, and streamline claims processing. The importance of telemedicine as a component of insurance coverage is also growing. This is particularly helpful during flu season because virtual care allows people to consult with clinicians while reducing the burden on medical facilities. According to the IMARC Group, the Unites States telemedicine market size is projected to exhibit a growth rate (CAGR) of 12.70% during 2024-2032. Moreover, technology is aiding transparency, with regulatory efforts emphasizing clear communication about plan benefits and costs. These innovations collectively enhance people’s trust and engagement.
U.S. Health Insurance Industry Segmentation:
IMARC Group provides an analysis of the key trends in each segment of the U.S. health insurance market, along with forecasts at the country and regional levels from 2026-2034. The market has been categorized based on provider, type, plan type, demographics, and provider type.
Analysis by Provider:
To get detailed segment analysis of this market Request Sample
- Private Providers
- Public Providers
A sizeable portion of the market is made up of private health insurance companies, which provide a variety of policies for individuals, families, and employer-sponsored groups. Major commercial insurers that together control a sizeable portion of the industry are included in this group. Common methods for private providers to differentiate themselves include specialized plans such as health maintenance organizations (HMOS), preferred provider organizations (PPOS), and high-deductible health plans paired with health savings accounts (HSAs).
Public health insurance providers, primarily consisting of government programs, play a vital role in ensuring coverage for vulnerable populations, including the elderly, low-income families, and children. Administered by state and federal agencies, these programs collectively cover millions of Americans and are a significant component of the broader U.S. healthcare system.
Analysis by Type:
- Life-Time Coverage
- Term Insurance
Lifetime coverage is a type of insurance plan that offers lifelong coverage as long as the premiums are consistently paid. Usually, these plans come with more extensive benefits, providing a mix of health insurance and occasionally including features that build up cash value as time goes on. Lifetime coverage is most appealing to individuals looking for security and steady premiums over the long term.
Term insurance in the context of health insurance refers to coverage that is granted for a predetermined amount of time, typically one to several years, and that needs to be renewed to continue. The cost and flexibility of this type of health insurance make it a popular choice for people who need temporary or extra coverage on top of their current employer-sponsored plans.
Analysis by Plan Type:
- Medical Insurance
- Critical Illness Insurance
- Family Floater Health Insurance
- Others
The most popular and basic kind of health insurance plan is medical insurance, which covers a wide range of medical services like doctor visits, hospital stays, surgeries, and preventative treatment. These policies provide policyholders with crucial protection against unforeseen medical costs and can be customized to cover both inpatient and outpatient treatments. Both public and private companies offer medical insurance policies, and they differ in terms of coverage networks, prices, and benefit levels.
A specific kind of health insurance plan called critical illness insurance is intended to offer financial assistance in the event that a serious illness, such as cancer, a heart attack, or a stroke, is diagnosed. Critical illness insurance, in contrast to typical medical insurance, provides a lump sum payout after diagnosis that can be used for anything, including paying for out-of-pocket medical bills, missed wages, or necessary lifestyle changes while recovering.
Family floater health insurance is a policy that provides coverage for all family members under one plan, with a common sum insured available for use by any member. This insurance type provides cost savings and convenience when compared to buying separate policies for each family member. Family floater plans are structured to offer thorough coverage for various services like hospitalization, maternity benefits, and preventive care, which are favored by young families and households with dependent children.
Analysis by Demographics:
- Minor
- Adults
- Senior Citizen
The aim of minor’s or children's health insurance plans is to provide comprehensive coverage that considers their specific medical needs. These plans often prioritize preventive treatments, essential for monitoring growth and development, and encompass regular check-ups, vaccinations, and wellness appointments. Emergency care, dental services, vision care, and specialists for children can be included as well.
A major portion of the market is made up of adults between the ages of 18 and 64. Adults usually have the option of getting health insurance through their employer, purchasing an individual policy on the marketplace, or qualifying for government programs such as Medicaid, based on their income and job situation. The requirements of this group range from maternity and reproductive health services to coverage for chronic conditions and preventive care.
Senior citizens primarily choose supplemental plans or plans offered by private insurers to expand their coverage. This demographic typically requires more specialized and extensive healthcare services, including management of chronic conditions, prescription drug coverage, and long-term care support. The rising need for geriatric care, home healthcare, and services for age-related conditions, such as Alzheimer’s and arthritis is also shaping the insurance products targeting this group.
Analysis by Provider Type:
- Preferred Provider Organizations (PPOs)
- Point of Service (POS)
- Health Maintenance Organizations (HMOs)
- Exclusive Provider Organizations (EPOs)
Preferred provider organizations (PPOs) are a popular market segment because they offer a flexible way to access healthcare providers. In addition to providing partial coverage for out-of-network procedures at higher rates, PPO plans enable policyholders to obtain care from a wide network of recommended providers without requiring referrals. Besides this, people who value convenience and choice when choosing medical professionals and facilities finds this kind of insurance appealing.
PPO and health maintenance organization (HMO) characteristics are combined in point of service (POS) plans, which are hybrid insurance models. By mandating policyholders to choose a primary care physician (PCP) who organizes treatment and makes referrals for specialized services, these plans strike a compromise between managed care and provider choice.
Health maintenance organizations (HMOs) are recognized for their ability to provide cost-effective services and organized care management. Individuals enrolled in HMO plans are required to select a primary care physician (PCP) who is responsible for managing their healthcare and giving recommendations for specialists within an established network.
Exclusive provider organizations (EPOs) have network requirements that are stricter compared to PPOs. EPO plans offer coverage solely for services obtained from providers within the network, unless it is an emergency situation. This insurance option offers a mix of affordability and freedom, typically with cheaper premiums compared to PPOs yet does not require referrals from a primary care physician like HMOs.
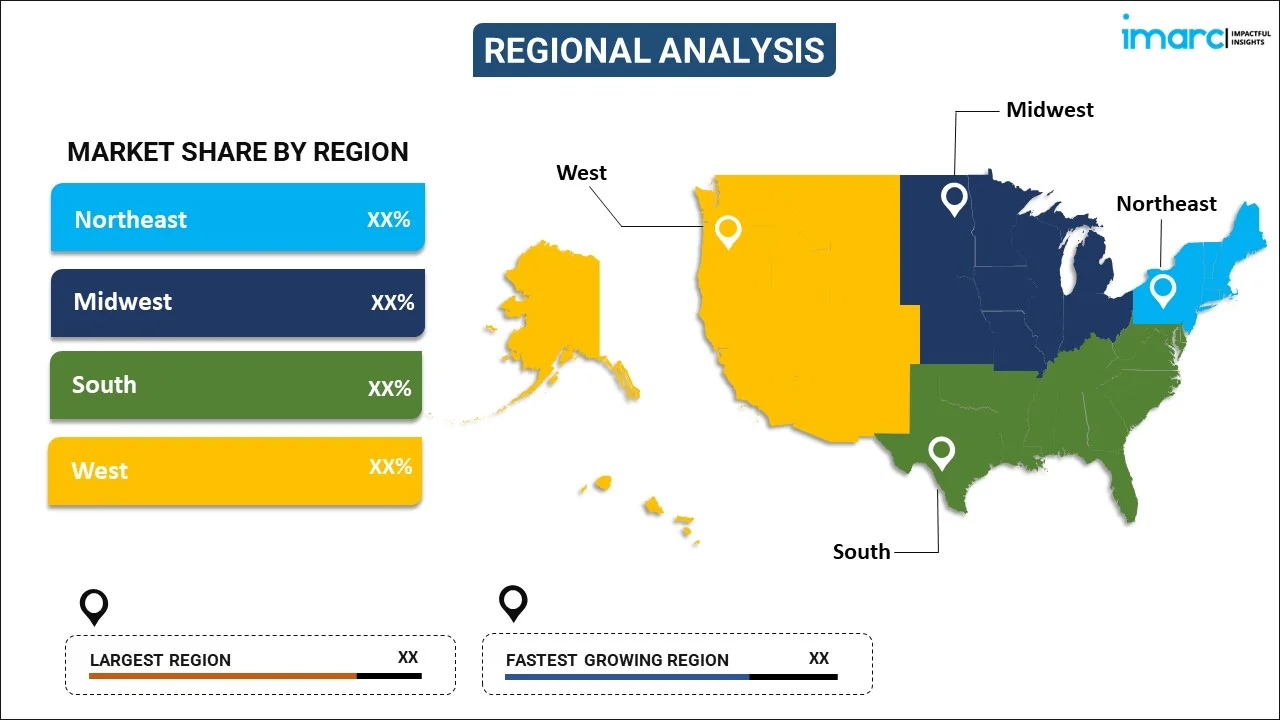
Regional Analysis:
To get detailed regional analysis of this market Request Sample
- Northeast
- Midwest
- South
- West
The Northeast area, containing states like New York, Massachusetts, and Pennsylvania, is at the forefront of health insurance innovation and has high rates of coverage. A major development in this area is the increase in public health programs and state-level efforts to attain nearly complete coverage. Furthermore, progress in digital health platforms is vital in the Northeast region, as insurance companies are introducing mobile apps and telehealth services to better serve the tech-savvy population and enhance healthcare accessibility.
The health insurance market in the Midwest, which includes Illinois, Ohio, and Michigan, is varied and influenced by both urban and rural factors. Since the Midwest has long struggled with rising healthcare expenses in relation to typical income levels, a major trend in this region is the emphasis on affordability and cost-containment strategies. In order to keep premiums affordable, insurers are reacting by providing more affordable high-deductible health plans (HDHPs) and cultivating alliances with nearby healthcare providers.
States like Georgia, Florida, and Texas are in the South. Due to disparate state policies and various degrees of Medicaid expansion, the region has long suffered with greater uninsured rates than other regions of the nation. To expand coverage alternatives, there is a growing shift toward private insurance products with more adaptable, short-term plans.
The Western region, which encompasses states like California, Washington, and Colorado, is at the forefront of progressive healthcare reform and technological integration within the insurance market. California, in particular, leads with state-specific policies that extend coverage and maintain patient protections. One significant trend in this region is the incorporation of innovative technologies such as AI-driven data analytics and comprehensive digital health platforms.
Competitive Landscape:
Key market players are actively adopting strategies to strengthen their market positions and enhance consumer engagement. A major focus is on expanding and integrating digital health solutions to improve service accessibility and user experience. Companies are investing in telehealth services, mobile apps, and data analytics tools to offer virtual consultations, personalized health tracking, and seamless claims processing. Partnerships and acquisitions are playing a major part in broadening service offerings and enhancing networks. For instance, Kaiser Permanente and Town Hall Ventures in 2024 announced the launch of Habitat Health, an organization designed to help older adults overcome the challenges of aging at home. If it is approved by the Centers for Medicare & Medicaid Services and the California Department of Health Care Services, Habitat Health plans to operate as a Program of All-Inclusive Care for the Elderly and support its participants to live independently in their homes and communities with better care and support.
The report provides a comprehensive analysis of the competitive landscape in the U.S. health insurance market with detailed profiles of all major companies.
Latest News and Developments:
- November 2024: UnitedHealthcare announced a significant expansion of its Individual & Family Affordable Care Act (ACA) Marketplace plans, now offering coverage in 30 states.This increase includes new coverage areas in Indiana, Iowa, Nebraska and Wyoming, as well as additional counties in 13 other states.
U.S. Health Insurance Market Report Scope:
| Report Features | Details |
|---|---|
| Base Year of the Analysis | 2025 |
| Historical Period | 2020-2025 |
| Forecast Period | 2026-2034 |
| Units | Billion USD |
| Scope of the Report | Exploration of Historical and Forecast Trends, Industry Catalysts and Challenges, Segment-Wise Historical and Predictive Market Assessment:
|
| Providers Covered | Private Providers, Public Providers |
| Types Covered | Life-Time Coverage, Term Insurance |
| Plan Types Covered | Medical Insurance, Critical Illness Insurance, Family Floater Health Insurance, Others |
| Demographics Covered | Minor, Adults, Senior Citizen |
| Provider Types Covered | Preferred Provider Organizations (PPOs), Point of Service (POS), Health Maintenance Organizations (HMOs), Exclusive Provider Organizations (EPOs) |
| Regions Covered | Northwest, Midwest, South, West |
| Customization Scope | 10% Free Customization |
| Post-Sale Analyst Support | 10-12 Weeks |
| Delivery Format | PDF and Excel through Email (We can also provide the editable version of the report in PPT/Word format on special request) |
Key Benefits for Stakeholders:
- IMARC’s industry report offers a comprehensive quantitative analysis of various market segments, historical and current market trends, market forecasts, and dynamics of the U.S. health insurance market from 2020-2034.
- The research report provides the latest information on the market drivers, challenges, and opportunities in the U.S. health insurance market.
- Porter's five forces analysis assists stakeholders in assessing the impact of new entrants, competitive rivalry, supplier power, buyer power, and the threat of substitution. It helps stakeholders to analyze the level of competition within the U.S. health insurance industry and its attractiveness.
- The competitive landscape allows stakeholders to understand their competitive environment and provides an insight into the current positions of key players in the market.
Key Questions Answered in This Report
Health insurance is a financial arrangement that covers the cost of medical expenses incurred by individuals or families. It provides access to healthcare services, including doctor visits, hospital stays, prescription medications, and preventive care, in exchange for monthly premiums. By reducing out-of-pocket costs, health insurance ensures affordability and protection against high medical bills, promoting overall financial and physical well-being.
The U.S. health insurance market was valued at USD 469.8 Billion in 2025.
IMARC estimates the U.S. health insurance market to exhibit a CAGR of 3.50% during 2026-2034.
The U.S. health insurance market is driven by rising healthcare costs, increased demand for comprehensive coverage, and growing adoption of private health insurance due to its customizable options. Technological advancements, including AI-powered tools and telemedicine, enhance accessibility and user experience. Additionally, the emphasis on preventive care, value-based care models, and wellness programs further propels market growth, addressing financial and health-related needs.
Need more help?
- Speak to our experienced analysts for insights on the current market scenarios.
- Include additional segments and countries to customize the report as per your requirement.
- Gain an unparalleled competitive advantage in your domain by understanding how to utilize the report and positively impacting your operations and revenue.
- For further assistance, please connect with our analysts.
 Request Customization
Request Customization
 Speak to an Analyst
Speak to an Analyst
 Request Brochure
Request Brochure
 Inquire Before Buying
Inquire Before Buying




.webp)




.webp)












